
Hematology Franchise: Update at 65th Annual Congress of the American Society of Hematology December 2023

Hematology Franchise Update 2 Statements contained in this presentation regarding matters that are not historical facts are “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995, as amended. Words such as "anticipates," "believes," "expects," "intends," “plans,” “potential,” "projects,” “would” and "future" or similar expressions are intended to identify forward-looking statements. Examples of these forward-looking statements include statements concerning: Keros’ expectations regarding its growth, strategy, progress and the design, objectives, expected results and timing of its preclinical studies and clinical trials for KER-050, KER-012 and KER-065, including its regulatory plans; and the potential of Keros’ proprietary discovery approach. Because such statements are subject to risks and uncertainties, actual results may differ materially from those expressed or implied by such forward-looking statements. These risks and uncertainties include, among others: Keros’ limited operating history and historical losses; Keros’ ability to raise additional funding to complete the development and any commercialization of its product candidates; Keros’ dependence on the success of its product candidates, KER-050, KER-012 and KER-065; that Keros may be delayed in initiating, enrolling or completing any clinical trials; competition from third parties that are developing products for similar uses; Keros’ ability to obtain, maintain and protect its intellectual property; and Keros’ dependence on third parties in connection with manufacturing, clinical trials and preclinical studies. These and other risks are described more fully in Keros’ filings with the Securities and Exchange Commission (“SEC”), including the “Risk Factors” section of the Company’s Quarterly Report on Form 10-Q, filed with the SEC on November 6, 2023, and its other documents subsequently filed with or furnished to the SEC. All forward-looking statements contained in this presentation speak only as of the date on which they were made. Except to the extent required by law, Keros undertakes no obligation to update such statements to reflect events that occur or circumstances that exist after the date on which they were made. Certain information contained in this presentation relates to or is based on studies, publications, surveys and other data obtained from third-party sources and the Company’s own internal estimates and research. While we believe these third-party sources to be reliable as of the date of this presentation, it has not independently verified, and makes no representation as to the adequacy, fairness, accuracy or completeness of, any information obtained from third-party sources. Finally, while we believe our own internal research is reliable, such research has not been verified by any independent source. The trademarks included in this presentation are the property of the owners thereof and are used for reference purposes only. Disclaimer

KER-065 therapeutic protein P R E C L I N I C A L Hematology Franchise Update 3 Focused on Transforming the Lives of a Wide Range of Patients with Disorders Linked to Dysfunctional TGF-β Superfamily Signaling We believe our product candidates have the potential to unlock the full therapeutic benefits of modulating the TGF-β superfamily and provide disease-modifying benefit to patients P H A S E 3P R E C L I N I C A L P H A S E 1 P H A S E 2 KER-050 therapeutic protein KER-050 therapeutic protein H E M A T O L O G Y KER-012 therapeutic protein P U L M O N A R Y & C A R D I O V A S C U L A R Myelodysplastic Syndromes (MDS) Myelofibrosis (MF) Pulmonary Arterial Hypertension Musculoskeletal 4 KER-012 therapeutic protein N E U R O M U S C U L A R Chronic Heart Failure with Preserved Ejection Fraction/Reduced Ejection Fraction Keros is a clinical-stage biopharmaceutical company Developing potentially differentiated product candidates designed to alter transforming growth factor-beta (TGF-β) signaling and target pathways critical for the growth, repair and maintenance of a number of tissue and organ systems Undisclosed Assets

B 4Hematology Franchise Update Clinical Presentations • “Durable Clinical Benefit with KER-050 treatment: Findings From an Ongoing Phase 2 Study in participants with Lower-Risk MDS” – Publication Number: 196 • “KER-050 Treatment Reduced Iron Overload and Increased Bone Specific Alkaline Phosphatase in participants with Lower-Risk MDS Supporting Potential to Restore Balance to the Osteohematopoietic Niche” – Publication Number: 1089 • “Modulation of TGF-β Superfamily Signaling By KER-050 Demonstrated Potential to Treat Myelofibrosis and Mitigate Ruxolitinib- Associated Cytopenia” – Publication Number: 3185 Preclinical Presentations • “RKER-050, A Modified Activin Receptor Type IIA Ligand Trap, Promoted Erythropoiesis in a Murine Model of Myelofibrosis” – Publication Number: 4524 • “RKER-216 Reversed Microcytic Anemia in a Mouse Model of Iron Refractory Iron Deficiency Anemia” – Publication Number: 2466 65th American Society of Hematology Annual Meeting and Exposition

B Imbalanced TGF-β Signaling in Bone Marrow Results in Ineffective Hematopoiesis and Poor Outcomes in Both MDS and MF1,2,3 Inhibition of Activin A may restore effective hematopoiesis and improve outcomes Poor Outcomes 1. Verma A, et al. J Clin Inv 2020; 2. Portale F, et al., Haematologica. 2019, 3. Rambaldi B., et al, Ann Hematol. 2021 BMP = bone morphogenetic protein; GDF = growth differentiation factor; TGF-β = transforming growth factor-β Myelosuppressive Ineffective Hematopoiesis Diseased Bone Marrow & Osteohematopoietic Niche Hematology Franchise Update 5

KER-050 is Designed to Target Bone Marrow Disorders of Ineffective Hematopoiesis Including MDS and MF Domain Effect Erythropoiesis ALL stages of differentiation and maturation Thrombopoiesis ALL stages of differentiation and maturation Bone Increased bone formation Iron Metabolism Improved iron utilizationFe KER-050 (elritercept) • Designed to inhibit select TGF- beta ligands, including Activin A, which has been associated with driving disease pathogenesis and progression Activins A+B 6Hematology Franchise Update

B KER-050 (Elritercept) 7 Investigational Treatment for Anemia and Thrombocytopenia in Patients with Myelodysplastic Syndromes Ongoing Phase 2 Clinical Trial of KER-050 for the Treatment of Anemia in Patients with Very Low-, Low- or Intermediate-Risk Myelodysplastic Syndromes Hematology Franchise Update

BHematology Franchise Update 8 MDS MDS is a collection of bone marrow disorders characterized by ineffective hematopoiesis and peripheral cytopenias. Clinical Consequences The clinical consequences of MDS include anemia, bleeding, iron overload, cardiovascular disease and progression to acute myeloid leukemia (AML). Survival Ranges Median survival ranges from approximately nine years for very low-risk patients to less than a year for high-risk patients. Scope In the United States, there are 60,000 to 170,000 patients living with MDS and 15,000 to 20,000 new cases of MDS reported each year. Myelodysplastic Syndromes (MDS) Progressive disease leading to AML and cardiovascular disease Cytopenias including severe anemia Severe fatigue and decreased QoL Impact of MDS Created with BioRender QoL = quality of life

Hematology Franchise Update 9 Current Treatment Landscape for Treatment of Anemia in Lower Risk MDS 1. Femaix P, et al. New Eng J Med 2020; 382:140-151 RBC Transfusions • ESAs are currently first line treatment of choice but response is limited in patients with endogenous erythropoietin levels (>200 U/L) and high transfusion burden (>4 units of RBC/8 weeks) Erythroid Maturation Agent Erythroid Stimulating Agents • RBC transfusions provide symptomatic relief of anemia • Transfusion dependency is associated with iron overload, further exacerbating damage to the bone marrow and increasing risk of AML progression and cardiovascular disease • Prolonged transfusion dependence is associated with shorter overall survival • Reblozyl approved in 1st and 2nd line MDS • In second line treatment, only 20% of high transfusion burden (HTB) patients achieved 8-week transfusion independence with Reblozyl® versus 4% with placebo1 • In 2nd line setting, “patient reported outcome (PRO) data showed no improvement in quality of life for patients who received luspatercept or who responded to luspatercept.” (Medical reviewer from the luspatercept FDA review document Page 11 4/3/2020) Unmet need remains for treatment that can address the multifaceted pathophysiology of MDS

BHematology Franchise Update 10 Data are presented as of a data cutoff date of September 1, 2023. RP2D = Recommended Part 2 Dose; CMML: chronic myelomonocytic leukemia; high transfusion burden (HTB): ≥4 units of RBC/8 weeks for hemoglobin (Hgb) ≤9 g/dL; low transfusion burden (LTB): 1-3 units of RBC/8 weeks for Hgb ≤9 g/dL; non- transfused (NT): Hgb ≤10 g/dL; RS = ring sideroblasts.; IO = Iron Overload; IC = Iron Chelation Ongoing Phase 2 Clinical Trial of KER-050 for the Treatment of Anemia in Patients with Very Low-, Low- or Intermediate-Risk MDS Part 2 Dose Confirmation Cohorts Part 1 Dose Escalation (completed N=31) A. LTB/HTB, RS+ N=30 B. LTB/HTB, Non-RS, N=30 C. NT, RS+ and Non-RS, N=10 D. CMML-0, N=10 E. LTB/HTB, with IO and IC, RS+ and Non-RS, N=15 F. LTB/HTB, with IO, no IC, RS+ and Non-RS, N=15 P ar ti ci p an ts in a ll P ar t 2 C o h o rt s in it ia te tr ea tm en t at R P 2 D Part 1 Extension (continued treatment at RP2D) Pretreatment Period 8 weeks Treatment Period 24 cycles, 96 weeks Follow-up Period 8 weeks Response data are presented for the modified intent to treat 24-week population (mITT24) that includes RP2D participants with at least 24 weeks of KER-050 treatment or who have discontinued (n=60) KER-050 administered subcutaneously once every four weeks (Q4W) Primary Objective: ▸ Assess safety and tolerability of KER-050 Key Eligibility Criteria: ▸ MDS per 2016 WHO criteria, RS+ or non-RS, very-low, low, or intermediate risk disease (LR-MDS) by IPSS-R with anemia (NT, LTB, HTB) ▸ CMML in Cohort D Select Efficacy Endpoints: ▸ IWG 2006 Hematological improvement-erythroid (HI-E): ▸ Hemoglobin increase of ≥1.5 g/dL for 8 weeks (in NT and LTB patients) ▸ Reduction of ≥4 RBC units transfused over 8 weeks compared to baseline (in HTB patients) ▸ Transfusion independence (TI) for at least 8 weeks in patients who require ≥ 2 RBC units transfused at baseline Ongoing Trial – Status as of Data Cutoff Date: ▸ Part 1 Extension Ongoing ▸ RP2D: 3.75 mg/kg with the ability to titrate to 5 mg/kg Q4W ▸ RP2D experienced patients: N=79 ▸ 7 (8.9%) patients received ≤3 doses ▸ 50 (63%) patients were ongoing and remained on treatment ▸ Median duration of treatment = Approx. 29 weeks (Range = Approx. 4 to 114 weeks) ▸ Median doses received = 7 (range 1 to 28 doses) ▸ 22 (27.8%) patients received ≥12 doses

B 11Hematology Franchise Update Trial Enrolled Hard-to-Treat Patients with High Disease Burden Data are presented as of a data cutoff date of September 1, 2023. *9 RP2D patients had missing baseline EPO; **Excludes 22 RP2D participants with unknown dysplasia category EPO= erythropoietin, SLD = single lineage dysplasia; MLD = multi lineage dysplasia Baseline Characteristic RP2D (N=79) Median age, years (range) 75 (53, 89) Sex, male, n (%) 50 (63.3) Hemoglobin, g/dL, median (range) 8.37 (3.7, 10.5) RS+, n (%) Non-RS, n (%) 57 (72.2) 22 (27.8) Prior ESA, n (%) 21 (26.6) Median baseline EPO level, U/L (range)* 127.8 (1, 4000) Thrombocytopenia, n (%) (platelets < 150 x 109/L) 20 (25) • 44 (56%) had high transfusion burden (HTB, ≥4 RBC units/8 weeks) • 25 (32%) heavily transfused (≥ 6 RBC units/8 weeks) • 50 (88%) had multi-lineage dysplasia (MLD) Baseline Transfusion Burden NT LTB HTB 19% (N=15) 25% (N=20) 56% (N=44) MLD 88% (N=50) SLD 12% (N=7) Baseline Dysplasia Category**

B 12Hematology Franchise Update KER-050 was Generally Well-tolerated • Most frequent TEAEs (≥ in 15% of patients) regardless of causality were: ▸Dyspnea or diarrhea (18; 22.8% each) ▸Fatigue (16; 20.3%) ▸Nausea (15; 19.0%) ▸Headache (12; 15.2%) • Most TEAEs were mild (Grade 1) to moderate (Grade 2) • 3 treatment-related TESAEs of injection site reaction (Grade 2), dyspnea (Grade 3), and syncope (Grade 3) occurred in 1 patient each ▸Dyspnea and syncope were assessed as not related to study treatment by the Sponsor due to underlying co-morbidities • Fatal TESAEs (cardiac failure and myocardial infarction) occurred in 2 (2.5%) patients; both were assessed as unrelated by the PI and Keros • No patients progressed to AML Category RP2D (N=79) n (%) Any TEAE 74 (93.7) Any treatment-related TEAE 33 (41.8) Any TESAE 28 (35.4) Any treatment-related TESAE 3 (3.8) Any TEAE leading to death 2 (2.5) Any TEAE leading to KER-050 discontinuation* 11 (13.9) Treatment-related = considered to be related to the study treatment by the treating investigator. Number and percent of patients with events were summarized. *Treatment-related TEAEs leading to KER-050 discontinuation: injection site reaction, platelet count increased, and dyspnea Unrelated TEAEs leading to KER-050 discontinuation: nodular melanoma, NSCLC, MI, dementia Alzheimer’s type, dyspnea, cardiac failure, and COPD & cardiac failure congestive (both in 1 patient) Data are presented as of a data cutoff date of September 1, 2023. AML = acute myeloid leukemia; COPD = chronic obstructive pulmonary disease; MI = myocardial infarction; NSCLC = non-small cell lung cancer; TEAE = treatment emergent adverse event; TESAE = treatment emergent serious adverse event

B Data are presented as of a data cutoff date of September 1, 2023. Hgb=hemoglobin; sTfR=soluble transferrin receptor 13Hematology Franchise Update KER-050 Treatment Led to Sustained Increases in Hemoglobin Observed Change in HgB, sTfR, and Ferritin Number of Patients • Durable increases in hemoglobin were achieved in NT and LTB patients • Increases in sTfR a marker of erythropoiesis and decreases in serum ferritin were also observed Collectively, suggests KER-050 resulted in durable restoration of erythropoiesis and improved iron metabolism

B Data are presented as of a data cutoff date of September 1, 2023. Hgb=hemoglobin; sTfR=soluble transferrin receptor 14Hematology Franchise Update Treatment of KER-050 Led to Decreased Iron Overload Regardless of Transfusion Burden in Exploratory Analysis Observed Change in Serum Ferritin by Baseline Ferritin • Among the 29 patients with baseline ferritin ≥ 1,000 and post-baseline measurements: • 14 (48%) showed decreases of ferritin to <1000 ng/ml while on treatment • 20 (69%) showed a ≥20% reduction in ferritin while on treatment • 2 patients, including one who was NT, discontinued iron chelator therapy due to decreases in ferritin observed while on treatment Number of Patients Supports KER-050 potential to ameliorate iron overload in patients with MDS, regardless of baseline transfusion burden

B Data are presented as of a data cutoff date of September 1, 2023. 1. Moses B, et al. ASH 2022; OHN=osteohematopoietic niche 15Hematology Franchise Update Potential of KER-050 to Restore Osteohematopoietic Environment in Exploratory Analysis • In MDS, disrupted crosstalk between hematopoietic stem cells and osteoprogenitors within the OHN leads to suppression of bone formation (osteogenesis) and hematopoiesis1 • BSAP (bone-specific alkaline phosphatase) is a marker of osteoblast activity • Sustained increase in BSAP observed with KER-050 treatment • Seen regardless of hematologic response, baseline transfusion burden, or RS status Observed Changes in BSAP Number of Patients Findings are consistent with preclinical studies and support KER-050’s potential to act on multiple components of the OHN to restore a bone marrow microenvironment conducive to functional hematopoiesis

B 16Hematology Franchise Update Hematologic Responses Observed in Broad Array of Patients Treated with KER-050 Responders/N (%) mITT24 All (N=60) HTB (N=33) Overall Responsea,b 30/60 (50) 15/33 (45.5) Modified IWG 2006 HI-Ec 28/60 (47) 15/33 (45.5) RS+ 23/40 (58) 12/23 (52.2) non-RS 5/20 (25) 3/10 (30) TI ≥8 weeksd 18/46 (39.1) 11/33 (33.3) RS+ 15/32 (46.9) 8/23 (34.8) non-RS 3/14 (21.4) 3/10 (30) Data are presented as of a data cutoff date of September 1, 2023. a. Includes data for weeks 0-24 in mITT24 patients; b. Defined as achieving modified IWG 2006 HI-E and/or TI; c. Modified HI-E = mean increase in hemoglobin ≥1.5 g/dL (NT+LTB) or reduction in transfusion of ≥4 RBC units (HTB) over 8 weeks on treatment compared to 8-week pre-treatment period; d. TI-evaluable patients received at least 2 RBC units in the 8-week pre-treatment period; mITT24 = modified intent to treat 24-week population; TI = transfusion independence HI-E and TI response rates in mITT24 patients with HTB were similar to those observed in the overall mITT24 population, supporting the potential for KER-050 to treat a broad array of patients with MDS including those with greater transfusion burden and bone marrow dysfunction

B 17Hematology Franchise Update Higher Hematologic Response Rates Observed in Patients with Baseline EPO <500 U/L • Studies in mainly LR-MDS patients suggest that the majority (~90%) of patients have serum EPO levels < 500 U/L1 • EPO levels ≥500 U/L are associated with lower erythroid response rates across multiple treatments1 • 9 patients in the mITT24 population had baseline EPO levels ≥ 500 U/L: • 6/9 had non-RS MDS • 3/9 were reclassified by IPSS-M as having high or very-high risk disease Data are presented as of a data cutoff date of September 1, 2023. a. Includes data for weeks 0-24 in mITT24 patients, excluding one patient with del5q MDS although their baseline EPO was <500 U/L; b. Defined as achieving modified IWG 2006 HI-E and/or TI; c. Modified HI-E = mean increase in hemoglobin ≥1.5 g/dL (NT+LTB) or reduction in transfusion of ≥4 RBC units (HTB) over 8 weeks on treatment compared to 8-week pre-treatment period; d. TI-evaluable patients received at least 2 RBC units in the 8-week pre-treatment period 1. Park, S et al. Annals of Hematology. 2020. Responders/N (%) mITT24 EPO<500 U/La All (N=50) HTB (N=26) Overall Responsea,b 28/50 (56.0) 14/26 (53.8) Modified IWG 2006 HI-Ec 26/50 (52.0) 14/26 (53.8) RS+ 21/36 (58.3) 11/20 (55) non-RS 5/14 (35.7) 3/6 (50) TI ≥8 weeksd 17/38 (44.7) 10/26 (38.5) RS+ 14/29 (48.3) 7/20 (35) non-RS 3/9 (33.3) 3/6 (50)

B TI ≥ 8 w ks TI ≥ 1 2 w ks TI ≥ 1 6 w ks TI ≥ 2 4 w ks TI ≥ 8 w ks TI ≥ 1 2 w ks TI ≥ 1 6 w ks TI ≥ 2 4 w ks 0 10 20 30 40 50 39 35 31 27 45 40 37 34 P e rc e n t o f P a rt ic ip a n ts 18Hematology Franchise Update Observed Rates of TI for ≥24 Weeks Support Durability of Response with KER-050 Treatment TI ≥ 8 w ks TI ≥ 1 2 w ks TI ≥ 1 6 w ks TI ≥ 2 4 w ks TI ≥ 8 w ks TI ≥ 1 2 w ks TI ≥ 1 6 w ks TI ≥ 2 4 w ks 0 10 20 30 40 50 33 27 24 21 39 33 30 28 P e rc e n t o f P a rt ic ip a n ts All HTB mITT24 Patients* mITT24 Patients*, EPO <500** Data are presented as of a data cutoff date of September 1, 2023. *During Weeks 0-48; **Excludes 1 patient with del5q MDS Durable TI was observed including in patients with HTB, and response rates were relatively higher in patients with baseline EPO < 500 U/L All HTB P e rc e n t o f P a ti e n ts P e rc e n t o f P a ti e n ts

B 19Hematology Franchise Update Durable TI Responses Observed with KER-050 Treatment 0 4 8 12 16 20 24 28 32 36 40 44 48 52 56 60 64 68 72 76 80 84 88 92 96100 0.0 0.2 0.4 0.6 0.8 1.0 Weeks P ro b a b il it y o f M a in ta in in g T I Duration of TI Response Number at Risk 18 18 18 15 14 13 13 9 7 7 7 6 6 6 6 5 4 3 3 3 3 3 2 2 1 0 • 18 participants in the mITT24 population had TI ≥ 8 weeks • 11/18 (61.1%) had HTB • 13/18 (72%) had TI ≥ 24 weeks • 11/18 (61.1%) had ongoing TI at time of data cut-off • Median baseline transfusion burden: 4 RBC units/8 weeks (range 2 to 11) • 6/11 (54.5%) had ongoing TI for > 52 weeks including participants who had received up to 11 RBC units/8 weeks at baseline • Median duration of response not reached (range: 8 to 98 weeks) Data are presented as of a data cutoff date of September 1, 2023. Longest TI interval through KER-050 treatment for mITT24 patients who achieved TI≥8 weeks during weeks 0-24; Patients with ongoing response censored at time of cutoff (denoted by vertical lines)

B 20Hematology Franchise Update Durable and Clinically Meaningful Improvements in FACIT-Fatigue Scores were Observed in TI Responders to KER-050 0 4 8 12 16 20 24 -10 -5 0 5 10 15 Week F A C IT - F T o ta l S c o re C h a n g e ( m e a n ± S E M ) TI ≥ 24 weeks Responder Non Responder 0 4 8 12 16 20 24 -10 -5 0 5 10 15 Week F A C IT - F T o ta l S c o re C h a n g e ( m e a n ± S E M ) TI ≥ 8 weeks Responder Non-Responder • Health-related quality of life (HRQOL) is negatively impacted by MDS1,2 with fatigue identified as a critically important domain to assess in patients with MDS3 • Prolonged transfusion dependence is associated with significantly worse HRQOL and shorter overall survival3 • Evidence suggests that worse fatigue is associated with reduced survival in MDS4 • The FACIT-Fatigue scale is a validated measure of self-reported fatigue and its impact upon daily activities and function that has been widely used in MDS studies4,5 Data are presented as of a data cutoff date of September 1, 2023. *Includes data for mITT24 patients with baseline FACIT-Fatigue scores (n = 1 missing) for TI ≥ 8 weeks Responder, assessed from Weeks 0 to 24; ** Includes data for mITT24 patients with baseline FACIT-Fatigue scores (n = 1 missing) for TI ≥ 24 weeks Responder, assessed from Weeks 0 to 48; 1. Stauder, R et. al., Blood. 2018; 2. Pleyer, Lisa, et al., Cancers. 2023; 3. Santini V. Et al., Clin Lymphoma Myeloma Leuk. 2018; 4. Oliva EN et al., Blood. 2021; 5. Sekeres M. et al., HemaSphere. 2023; MCID = minimally clinically important difference * ** MCID = 3 MCID = 3

B Data are presented as of a data cutoff date of September 1, 2023. 1. Madry et al, Br J Haematol 2022; 2. Oliva E, et al. Am J Blood Res 2011; 3. Gatterman N Int J Hematol 2018; 4. Yndestad A J Appl Physiol. (2009) 106:1356–64; 5. Liu H et al Arteriosclerosis,Thrombosis, and Vascular Biology. 2023;43:330–349; 6. Phillips D, et al. Cytokine Growth Factor Reviews 2009; 20(2):153-164; 7. Ryanto G, et al. Int J Mol Sci 2023; 24(4), 3332; 8. Lin JF, et al. Acta Cardiol Sin 2016; 32(4):420-427; 9.Yndestad et al Circulation. 2004;109:1379–1385; 10. Roh et al Sci Trans Med 2019; CVD=cardiovascular disease; NT-proBNP=N-terminal prohormone brain natriuretic peptide 21Hematology Franchise Update Potential of KER-050 to Reduce Cardiac Stress in Exploratory Analysis • In patients with LR-MDS, cardiovascular (CV) events represent a major cause of death possibly due to myocardial stress exacerbated by chronic anemia and iron overload in MDS1-3; NT-proBNP is a biomarker of myocardial stress • Activin A has been shown to play a pathophysiologic role in CVD4,5, and has been associated with inflammation6, vascular and myocardial remodeling7,8, myocardial infarction9 and severity of HF10 • Decreases in NT-proBNP were observed rapidly following initiation of dosing and were sustained for the majority of individuals regardless of erythropoietic response Observed Decreases in NT-proBNP Suggests KER-050 may ameliorate cardiac strain directly via inhibition of activin A and indirectly by improving anemia and reducing transfusion burden

B 22Hematology Franchise Update Summary of KER-050 in MDS • In the ongoing Phase 2 clinical trial of KER-050 in LR-MDS, the majority of patients enrolled had HTB or MLD indicating a difficult-to-treat trial population • KER-050 was generally well-tolerated as of the data cut-off date, with a safety profile consistent to that previously reported for this trial1,2 • Durable responses of transfusion independence were observed in a broad range of patients with LR-MDS, including those with HTB • Analysis of patients with EPO < 500 U/L revealed improved erythroid responses across the trial population, including in patients with HTB or non-RS disease • Transfusion independence, increases in hemoglobin, and increases in platelets were observed, supporting the potential for KER-050 to ameliorate ineffective hematopoiesis across multiple lineages in patients with MDS • Patients who achieved transfusion independence showed clinically meaningful improvements in FACIT-Fatigue scores indicating potential for KER-050 to improve quality of life in patients with LR-MDS • Observations from exploratory assessments of biomarkers: • Sustained increases in bone specific alkaline phosphatase (BSAP) were observed with KER-050 treatment supportive of potential to improve the bone marrow microenvironment • Several patients presented with elevated NT-proBNP at baseline, suggestive of increased myocardial stress • Rapid decreases with NT-ProBNP were observed with KER-050 treatment in HI-E/TI responders and non-responders • Collectively, these results support advancing KER-050 into a Phase 3 registration trial in patients with LR-MDS 1 Giagounidis et al. EHA 2023; 2 Chee et al. ASH 2022

B KER-050 (Elritercept) 23 Investigational Treatment for Anemia and Thrombocytopenia in Patients with Myelofibrosis Ongoing Phase 2 Open-Label Clinical Trial to Evaluate the Safety and Efficacy of KER-050 as Monotherapy or in Combination with Ruxolitinib in patients with Myelofibrosis Hematology Franchise Update

Hematology Franchise Update 24 Myelofibrosis MF MF is a rare cancer of the bone marrow in which the marrow is replaced by scar tissue and is not able to produce healthy blood cells Current Treatments Currently, there are limited therapeutic options to address the MF-associated cytopenias. Patients not only often experience multiple disease-associated, but also treatment-emergent, cytopenias, including anemia and thrombocytopenia Scope In the United States, there are 16,000 to 18,500 patients living with MF and approximately 3,000 newly diagnosed each year Clinical Consequences MF is characterized by ineffective hematopoiesis, an enlarged spleen, bone marrow fibrosis and shortened survival. Both anemia and thrombocytopenia are negative prognostic indicators Impact of MF Progressive disease leading to splenomegaly, bone marrow fibrosis and AML Cytopenias including treatment and disease related severe anemia Severe fatigue and Decreased QoL Created with BioRender

BHematology Franchise Update 25 Primary Objective: ▸ Part 1: Assess safety and tolerability of KER-050 ▸ Part 2: Confirm safety and tolerability of the dose(s) selected from Part 1 Secondary Endpoints include: ▸ Evaluate the pharmacokinetics, pharmacodynamics and efficacy of KER-050 administered with or without ruxolitinib Ongoing Phase 2 Clinical Trial to Evaluate KER-050 as Monotherapy or in Combination with Ruxolitinib in Patients with MF Following recommendation by the Safety Review Committee, dosing for Part 2 of this trial was initiated at a starting dose of 3.75 mg/kg, with an opportunity to dose escalate to 5.0 mg/kg based on individual titration rules, in both combination and monotherapy arms

B • Patients with high disease burden and severe erythropoietic dysfunction • Most receiving transfusions • 37% TD (IWG 2013 criteria; ≥6 RBC units/12 weeks) • Transfusions prevalent even among NTD (median: 3 RBC units/12 weeks) • Most had splenomegaly • Marked splenomegaly observed in the KER-050+RUX arm, indicative of inadequate control of disease • TD and NTD had anemia with EPO erythropoietic dysfunction • In TD, mean serum EPO was 543 IU/L and in NTD, mean EPO was 325 IU/L 26Hematology Franchise Update Baseline Characteristics RESTORE Baseline Demographics RESTORE Baseline Biomarkers of Erythropoiesis Data are presented as of a data cutoff date of September 14, 2023. IWG=International Working Group; LLN=lower limit of normal; RUX=ruxolitinib; ULN=upper limit of normal

B 27Hematology Franchise Update KER-050 Was Generally Well-Tolerated in Patients with Significant Disease Burden • TEAEs mild to moderate • Treatment-related TEAEs relatively infrequent • Two had Grade 3 or higher worsening cytopenias • One Dose Limiting Toxicity in Part 1 • Increased Hgb ≥2 g/dL in dose Level 2 cohort of monotherapy arm • No associated AE, Hgb within normal limits • Three TEAEs* leading to death, all deemed unrelated to study therapy Data are presented as of a data cutoff date of September 14, 2023. *Transformation to AML, cerebrovascular accident and pneumonia DLT=dose limiting toxicity
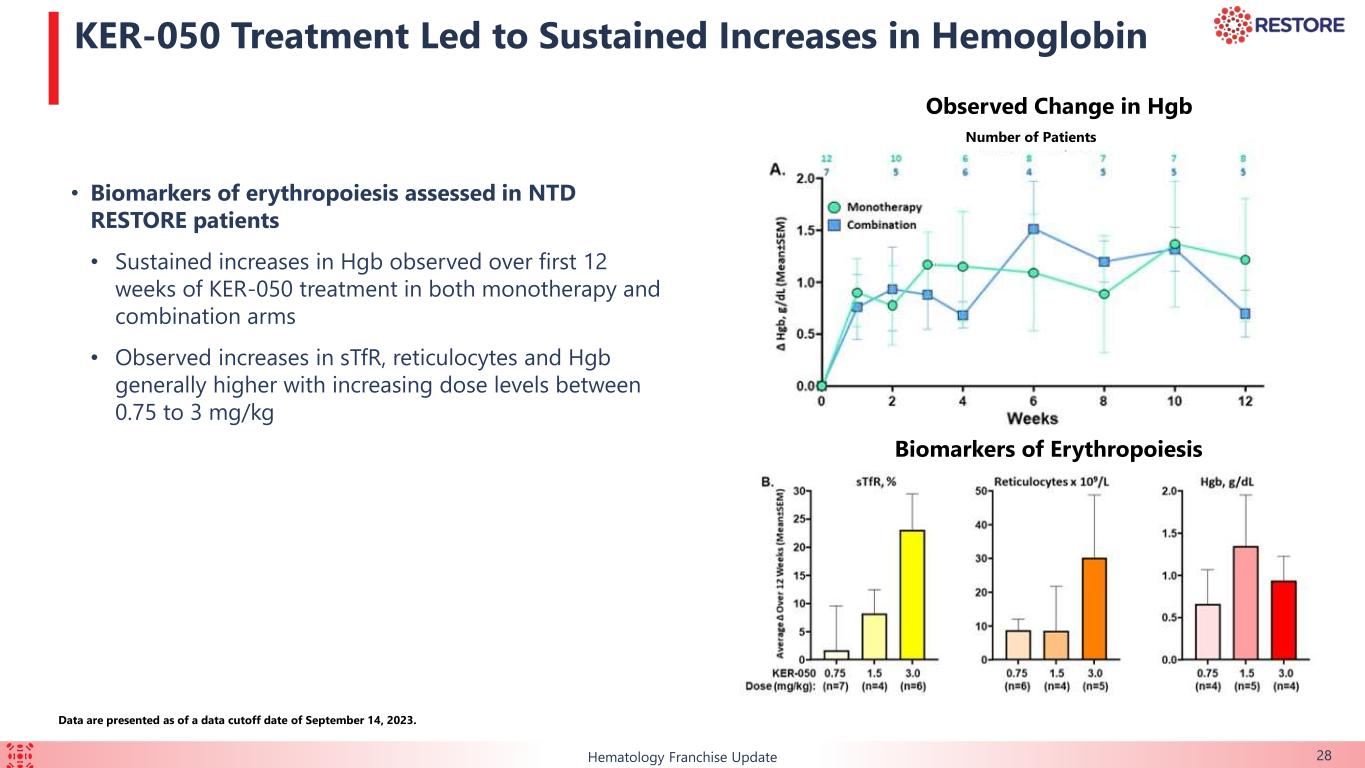
B 28Hematology Franchise Update KER-050 Treatment Led to Sustained Increases in Hemoglobin • Biomarkers of erythropoiesis assessed in NTD RESTORE patients • Sustained increases in Hgb observed over first 12 weeks of KER-050 treatment in both monotherapy and combination arms • Observed increases in sTfR, reticulocytes and Hgb generally higher with increasing dose levels between 0.75 to 3 mg/kg Number of Patients Biomarkers of Erythropoiesis Observed Change in Hgb Data are presented as of a data cutoff date of September 14, 2023.

B 29Hematology Franchise Update Treatment with KER-050 Led to Robust Increases in Hemoglobin and Reduction in Transfusion Burden in MF Patients • Hemoglobin assessed in NTD RESTORE patients: • Observed increases in Hgb in monotherapy arm suggests potential for KER-050 to address anemia due to underlying MF • Observed increases in Hgb in combination arm suggests potential to mitigate RUX-associated anemia Data are presented as of a data cutoff date of September 14, 2023. Observed Maximum Change in Hgb: NTD Patients Observed Reductions in Transfusion Burden • Changes in transfusion burden over 12 weeks assessed in patients receiving ≥ 3 units RBC/12 weeks at baseline • Decreased transfusion burden occurred in most patients, notably: • At 3 lowest KER-050 dose levels • In patients receiving up to 15 RBC units/12 weeks at baseline • Data support potential of KER-050 to improve anemia due to MF and RUX-associated anemia 1 1 2 2

B 30Hematology Franchise Update Preliminary Data Support Potential for KER-050 to Address Multiple Aspects of MF Hematopoiesis Spleen Size Symptoms • Observed increases in markers of erythropoiesis • Mean increases in hemoglobin and reduction in transfusion burden observed over 12 weeks • Maintenance or improvement in platelet counts observed • Observed reduction in spleen size in 4/7 (57%) evaluable* patients (1/3 mono, 3/4 combo) at Week 24 • Median reduction (n=4) = -27.1% (range -47.5% to -11.2%) • Median change (n=7) = -11.2% (range: -47.5% to 30%) • Observed reduction in disease symptoms in 8/12 (67%) evaluable# patients at Week 24 • Median reduction (n=8) = -16.8% (range -55.6% to -6.7%) • Median change (n=12) = -13.2% (range -55.6% to 54.5%) Data are presented as of a data cutoff date of September 14, 2023. *Evaluable defined as patients with baseline spleen size ≥ 450 cm3 and a Week 24 spleen assessment # Evaluable defined as patients with at least 2 symptoms with an average score ≥ 3 or an average total score of ≥ 10 on the MF-SAF-TSS questionnaire at baseline and with a Week 24 MF-SAF-TSS assessment

B 31Hematology Franchise Update Summary of KER-050 in Myelofibrosis • KER-050 was generally well-tolerated in RESTORE Part 1 as of the data cutoff date, including patients with high disease burden and complex comorbidities • Safety review committee approved RP2D of KER-050 consistent with dose selected for Part 2 of the ongoing Phase 2 clinical trial of KER-050 in patients with lower-risk MDS • RESTORE data presented here support potential for KER-050 to: • Ameliorate ineffective hematopoiesis and address cytopenias (anemia and thrombocytopenia) due to MF and associated with RUX • Based on observed increased markers of erythropoiesis, increased Hgb, decreased transfusion burden, maintained or increased platelets even at doses <RP2D • Provide broader clinical benefit in patients with MF (decreased spleen size and improved symptoms)

B •KER-050 is a novel ligand trap designed to inhibit select TGF-beta ligands, including Activin A, which has been associated with driving disease pathogenesis and progression •Data presented at ASH from the Phase 2 trials in MDS and MF support the potential of KER-050 to ameliorate ineffective hematopoiesis, improve bone health and reduce cardiac stress • In LR-MDS patients: • KER-050 demonstrated durable transfusion independence, including in patients with high transfusion burden • Durable clinical responses were associated with improvements in patient-reported measures of fatigue • Exploratory biomarker data demonstrate the potential of KER-050 to reduce NT-proBNP, a measure of cardiac stress/strain, and other key biomarker data, supporting its broad potential •Collectively, these results support advancing KER-050 into a Phase 3 registration trial in patients with LR-MDS • Keros plans to engage with regulators in H1 2024 on the design of the Phase 3 clinical trial of KER-050 in patients with LR-MDS • In MF: • Preliminary findings from Phase 2 clinical trial in myelofibrosis demonstrate that KER-050 can ameliorate ineffective hematopoiesis and address cytopenias • KER-050 has the potential broader clinical benefit seen through reduction of spleen size and overall reduction in symptom score 32Hematology Franchise Update Key Takeaways

Q&A